 Note: Originally published May 15, 2020
Note: Originally published May 15, 2020
It is easy to be confused and overwhelmed by the ever-changing landscape of the novel coronavirus pandemic and what it has wrought.
We are living our lives as never before. And just when you think you have a handle on your everyday conduct – doing things like responsibly social distancing, getting your food via delivery, and handling health care over the telephone or via video conferencing – the rules change again, as happened recently when the state of Georgia relaxed restrictions on “non-essential businesses.” And then the questions start again…
- What is the right thing to do, and what can I trust?
- Have we “flattened the curve,” and is the worst behind us?
- How can I best stay healthy; should I just start going about my normal routines as much as possible?
Longstreet Clinic physicians Andrew Reisman, M.D., a family medicine specialist who is also the current president of the Medical Association of Georgia and sits on Governor Brian Kemp’s COVID-19 task force, as well as Hall County’s COVID task force, and Erum Farooqi, M.D., an internal medicine specialist, want you to know that it is perfectly normal to wonder all of these things and more. Below, they answer some commonly asked questions about the virus based on what medicine now knows about this unprecedented health situation in hopes this information will help you make decisions as parts of the state begin to reopen.
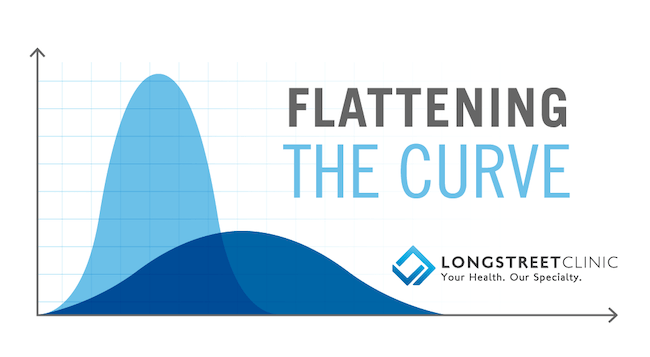
We hear so much about “flattening the curve,” what does that actually mean? And have we, in fact, achieved that?

Dr. Farooqi: In reference to COVID-19, “Flattening the curve” is a term used in epidemiology to refer to the spreading of the projected number of new cases over a longer period of time, rather than having a sharp spike in cases. “Flattening the curve” is an attempt to slow the spread of the virus enough to ensure that there are not too many sick patients at any given point in need of medical assistance. This allows the health care infrastructure to be able to care for them steadily and effectively without panic or compromise. “Flattening the curve” keeps our hospitals from becoming overwhelmed, rationing care, and allows our doctors and nurses to better treat those in need of serious medical attention.
Dr. Reisman: Looking at the numbers from Northeast Georgia Health System’s daily updates, it appears we did a good job in March and April of taking precautions and slowing the spread so that critical care bed usage remained at 60 to 80 percent and ventilator usage under 40 percent. We have seen models that show our local caseload may continue to rise into June, and NGHS was projecting that it will reach staffing capacity by late May. Hopefully, those predictions don’t come to pass, and we will have more capacity due to patients hospitalized in March or April being discharged.
Considering those realities, does that mean the worst is behind us – even with the state of Georgia loosening restrictions on non-essential businesses and opening beaches for limited public use?

Dr. Farooqi: It remains to be seen what will happen following the recent relaxation of statewide guidelines. The reality is that it will take weeks to really know if the reopening of the economy will lead to a second surge. Labeled an emerging “hot spot,” Hall County has already experienced an elevated rate of growth as compared to other counties and currently has its highest number of cases yet. The good news, however, is that testing has continued to increase here in Hall County. Theoretically, this means better detection and containment of cases as they emerge, a process that could, hopefully, dampen a potential second surge.
Dr. Reisman: Once we started to understand it (the novel coronavirus and COVID-19, the disease it causes), we have seen that we misestimated some aspects of it. In short, I think we grossly underestimated the number of people that are and have been infected and overestimated the number of people that would present with severe symptoms. That being said, this is still a very dangerous virus that everyone should be aware of, as it can take anyone with chronic health issues and destabilize their health condition; and we’ve all seen it can be very deadly for anyone over 60. No one should be casual about this. We urge everyone to still take precautions wherever possible, including social distancing and wearing protective equipment such as masks and gloves.
Am I safe to resume being around people outside of my immediate family and resume going to the businesses that have re-opened?

Dr. Reisman: Everyone has to determine their own level of risk. And you have to be respectful of others and be responsible. Do not go hang out with a bunch of other people if you know you will be going home to be around elderly family members. Or, if you’re a teenager, you have to think that, just because you might not get sick that it is still dangerous. For instance, you could get it and spread it to your parents and make them severely ill. It is all about making the wisest decision for yourself and your family based on the knowledge we currently have. Of course, there will be a risk of contracting COVID-19 if you are around other people more often. But you can do things to help minimize that risk, such as wearing a mask and gloves.
Dr. Farooqi: This virus is not going anywhere anytime soon. So, ideally, until we have a vaccine and a vigorous vaccination program in place, it’s best to continue the increased sanitary and hygiene practices we have hopefully become proficient at – as well as continuing social distancing guidelines and staying at home as much as possible. However, we also know that these guidelines may not be possible for everyone in this time of economic hardship. And though it may seem like we are having to choose between life and livelihood, there are measures that we can undertake to mitigate our risk as we return to the workforce. And we really should wear masks whenever we are in public.
If I am considering re-opening my business, what steps can I take to minimize the risks of myself, employees or customers contracting COVID-19?
Dr. Reisman: If you are re-opening your business in any shape, form or fashion you need to do your best to ensure that yourself and employees and customers maintain the best social distancing practices that you can – for restaurants that means not sitting people at tables right next to each other (perhaps leave a table open in between every diner). Also, keep surfaces wiped down and clean (with soap, bleach or alcohol-based cleansers).
Dr. Farooqi: To minimize the impact of COVID-19 on both employees and customers (and thus the general public), it is important that all employers plan appropriately and thoroughly to prevent a cascade of potential failures. Here are some references where you can find detailed guidance to prevent workplace exposures to COVID-19:
What do we currently know about the novel coronavirus?
Dr. Farooqi: SARS-CoV-2 is the virus that causes COVID-19 infection. It originated and spread from China to many other countries around the world, including the United States. We are continually learning more about its manifestations, however, what is concrete is that it can cause a multitude of illness ranging from mild to severe and, in some cases, even death.
Most infected/infectious patients will be asymptomatic – that is show no visible symptoms – or only experience mild symptoms and then recover. These symptoms (albeit an evolving list) include fever, chills, cough, shortness of breath, loss of taste and smell, nausea, vomiting and diarrhea. There is also new data suggesting that there are other emerging non-respiratory symptoms such as blood clots, strokes and rashes. Even though there has been a recent discovery of multisystem inflammatory syndrome (MIS-C) in children as young five, this virus mostly afflicts the elderly, male gender, and those with underlying health issues – such as diabetes, cardiovascular disease (high blood pressure, high cholesterol, congestive heart failure) and the obese.
According to the CDC, symptoms of COVID-19 may appear in as few as two days or as long as 14 days, but it is generally assumed to be around five days after exposure. During this time when there are no symptoms, infected individuals may unknowingly spread the virus.
Transmission of SARS-CoV-2 virus occurs through droplets, aerosol transmission and physical contact. Droplet transmission occurs via respiratory droplets produced when an infected person speaks, coughs or sneezes. Those droplets are then inhaled by another person in close proximity to the infected patient. Aerosol transmission occurs when respiratory droplets containing the virus mix into the air and stay suspended in poorly circulated air for an extended period of time (this may happen due to sneezing, breathing treatment or intubations). Once aerosolized, the virus may be inhaled by someone occupying or moving through the same space. Contact transmission occurs when a person touches a contaminated surface and then inadvertently touches his or her mouth, nose, or eyes.
Rough estimates are that the SARS-CoV-2 virus remains stable for up to 24 hours on cardboard, two-three days on plastic and stainless steel and up to three hours in aerosols, including fog, mist, dust, air pollutants, and smoke. Therefore, it is possible to get infected through inhalation and by touching contaminated objects and then inadvertently touching your ear nose, mouth or eyes.
With all of that in mind, what is the safest course of action for me and my family?
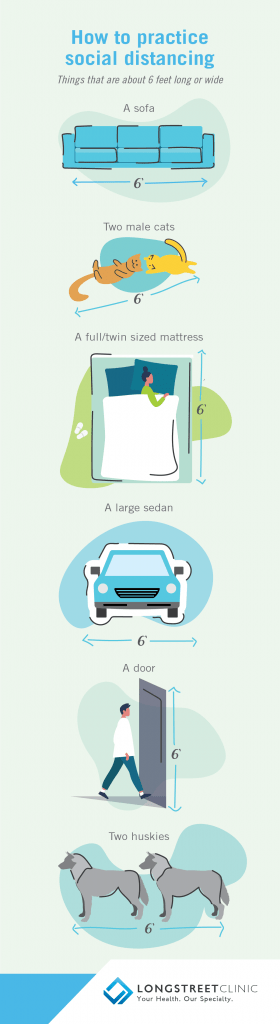 Dr. Reisman: Everybody should continue do the right thing for themselves, their family and for the good of the entire state and nation. That means you need to immediately quarantine yourself if you have ANY symptoms and/or you think you may have COVID-19 – and be sure to contact a healthcare professional to seek their help and advice. Also, if you are in a higher-risk group – in other words you are over 60, have a chronic illness such as COPD, heart disease, etc., have an auto-immune deficiency, are under treatment for cancer, etc. – then make sure you maintain social distance practices. Don’t be around anyone that you feel is at risk for exposure at any time.
Dr. Reisman: Everybody should continue do the right thing for themselves, their family and for the good of the entire state and nation. That means you need to immediately quarantine yourself if you have ANY symptoms and/or you think you may have COVID-19 – and be sure to contact a healthcare professional to seek their help and advice. Also, if you are in a higher-risk group – in other words you are over 60, have a chronic illness such as COPD, heart disease, etc., have an auto-immune deficiency, are under treatment for cancer, etc. – then make sure you maintain social distance practices. Don’t be around anyone that you feel is at risk for exposure at any time.
Dr. Farooqi: Balancing the needs and health of your family is no doubt a daunting task. There are no simple or easy answers here. Every family’s needs are unique and there are many variables to be considered when planning a safe course of action – such as childcare (or even eldercare), job security concerns or dealing with job loss and financial hardship. Then there is your personal health risk, which depends on your pre-existing health conditions, age, and the health risk to those whom reside with you. Bearing these factors in mind, you’ll have to try to make an informed and individual decision based on what’s best for you and your family and how much risk you’re willing to safely tolerate in exchange for the benefit that the action may provide to yourself and your family. It remains imperative that those highest at risk should exercise an additional level of caution right now – these include the elderly, and individuals with underlying health conditions such as diabetes, or cardiovascular disease.
As with everything in life, risk should not outweigh the potential benefit. There should always be calculated caution when there is risk. So, we must try to continue to wear masks and maintain social distancing as much as possible to protect ourselves, our families and the public at large, despite governmental relaxation in a bid to boost the economy. If you do decide to resume visiting friends or family, it would be much safer to socialize outdoors (such as patios, backyards, driveways, etc.) where there is better ventilation, direct sunlight and more space to spread out. These measures won’t completely stop virus transmission but will certainly reduce it.
If I have any questions about my health or my family’s health during this pandemic what is the best course of action?
Dr. Reisman: With the advancements we have made in technology, like telehealth, there is no reason you should not receive sound health care, no matter what is happening in your life. Thanks to the dedication of our technology team, doctors, nurses and management at the Longstreet Clinic, we have been able to maintain the level of medical care our patients have come to expect, even during the pandemic. So, if you have any questions about how you’re feeling or health situation, the first step is for you to contact your care providers over the phone or via MyChart and seek their advice. If you are feeling extremely ill, please do not wait. Contact your doctor right away. And if you have ANY trouble breathing you should always go to the emergency room, no matter if you have or think you may have COVID-19 or not.
Dr. Farooqi: Of course, always refer to the CDC website, which serves as an extensive source of all kinds of helpful information and recommendations. We want you to know that we will always be here to care for you should you need us at Longstreet Clinic. Rest assured, we offer the safest clinical environment possible and will ensure that, if you do have to come in for an appointment, that you will be seen under the safest circumstances possible. And our telehealth options can also provide great healthcare without the concerns of a trip to the office.
For more information about enhanced screening protocols on our campuses, click here.
For more resources related to COVID-19 from Longstreet Clinic, click here.
